[Baltimore Sun] Want to slim down? Change your lifestyle, not your medication | GUEST COMMENTARY
The newer oral and injectable weight loss drugs that are sweeping the developed world seem at first glance to be the long-sought answer to the ever-growing crisis of an overweight and obese population. As a physician with over 40 years of experience with patients and their illnesses, I am confident that — except in selected cases — these drugs are not the best approach to this problem.
To understand the scope of the problem itself, we need to look at the facts. In our own country, the prevalence of individuals who are either overweight or obese (defined as a body mass index of greater than 25 and 30, respectively) is approaching 75%. The average adult male in the United States weighed 166 pounds in the 1960s. Today that number is 200 pounds. One in three American adults is prediabetic, and 80% of them do not even know it.
Ultra-processed food, which makes up about 58% of our diet, is leading us down a path of chronic illness and disability. This, combined with a populace that is more sedentary than at any time in history, is creating a population of people at higher risk of developing chronic cardiovascular, autoimmune, joint, respiratory, sleep-related, neoplastic (cancer) and other diseases that will severely strain our already overburdened health care system. Within the next 10 years, there will be more people over the age of 65 than under the age of 18 in this country. These older and sicker Americans will suffer further from the looming shortage of doctors, nurses and other health care workers, and, as we continue to throw money at the problem (about 20% of our yearly federal budget goes to health care), the situation will eventually become untenable.
Yet we cling to medications, instead of lifestyle changes, for the answer to our ills. Twenty percent of Americans take five or more prescription medications, and 85% are on at least one prescription medication. We are a heavily dosed populace.
Now that certain oral and injectable drugs have been shown to take weight off quickly and dramatically in a large number of patients, people can’t seem to get enough of them. But do we really know the long-term ramifications of these agents? What does the science show?
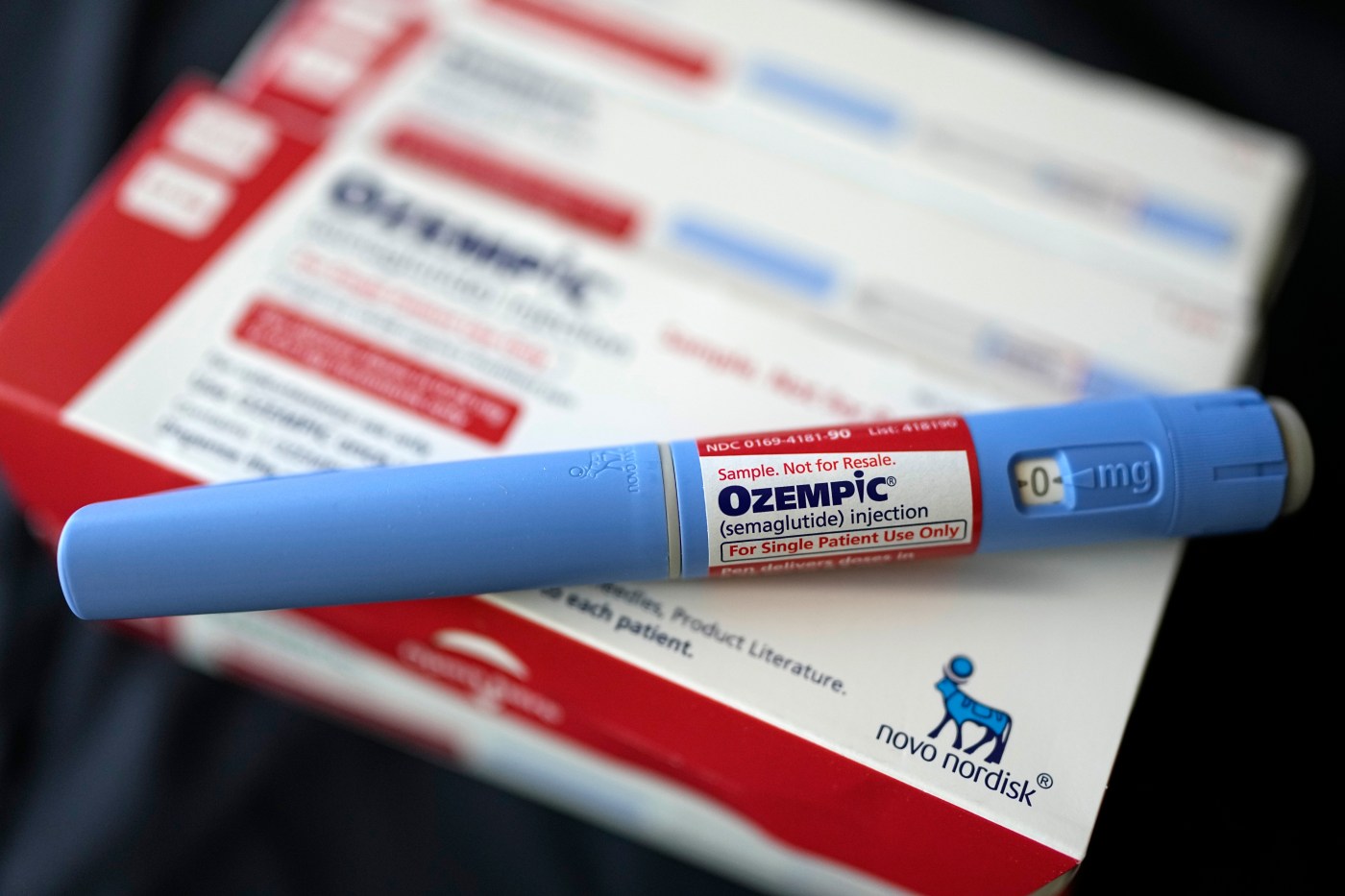
These newer medications, like Jardiance (empagliflozin), Monjauro (tirzepatide), Ozempic and Wegovy (both semaglutide) were originally designed to help people with type 2 diabetes and related co-morbidities (concurrent illnesses). But then doctors began using them off-label to take weight off and then things really got hot for them. Patients, whether 15 or 150 pounds overweight, clamored for them. And therein lies the problem.
In patients who are significantly overweight and have co-existing cardiovascular illnesses, these drugs have been proven to be beneficial, as evidenced by a November article in The New England Journal of Medicine that revealed a reduction in cardiovascular-related deaths when patients used the drug semaglutide versus placebo.
But in patients who desire to lose a small or moderate amount of weight, is it really worth the risks that have emerged in recent studies? There have been reports, such as the one from October published in the Journal of the American Medical Association from The University of British Columbia. It linked GLP-1 agonists (Monjauro and Zepbound are in this class) to a nine times higher incidence of pancreatitis, an over four times the risk of bowel obstruction and a 3.67 times the risk of gastroparesis (stomach paralysis) when compared to using weight loss treatment bupropion and naltrexone.
Then there’s the cost, which can run to about $1,200 a month for these agents and is often not covered by insurance. Combine this with the fact that many patients must remain on the drugs indefinitely, because the weight just comes back on with a vengeance if the drugs are stopped.
Unless we have a cultural change regarding how we eat, how we use (or don’t use) our bodies, and the way we approach medication as a crutch for our poor habits, we will never make a dent in the poorer health outcomes we have despite spending more money on health care than many other Westernized countries combined. The coming shortage of doctors and nurses, along with spiraling health care spending, will force us to a reckoning that will shock many in the near future.
Dr. David Sherer (www.drdavidsherer.com) is a retired physician and writer. His latest book is “Hunger Hijack, How Your Eating Habits are Changing Your Brain and Making You Sick” (Armin Lear Press, April 2024)
